 Michael Wang, MD, a renowned spine surgeon at the University of Miami Health System, is one of the pioneers in advancing the use of minimally invasive techniques to perform lumbar fusions.
Michael Wang, MD, a renowned spine surgeon at the University of Miami Health System, is one of the pioneers in advancing the use of minimally invasive techniques to perform lumbar fusions.
Dr. Wang’s latest achievement is an "awake" minimally invasive surgical (MIS) transforaminal lumbar interbody fusion (TLIF), which he performs with a new long-acting, local infiltration analgesic called EXPAREL (liposomal bupivacaine). Dr. Wang administers the analgesic in the paraspinal muscles and skin to allow the patient to have minimal postoperative pain after the TLIF is performed.
Dr. Wang is among the first surgeons to publish outcomes data comparing open lumbar fusion surgery to minimally invasive surgery.1 "My data was able to quantify the value of MIS TLIF over traditional open methods, in terms of shortening hospital stays and lowering the acute costs of hospitalization," he says. "In addition to the inherent benefits of minimally invasive surgery such as smaller incisions, less soft tissue injury, and reduced blood loss, we can also treat pain differently using a non-narcotic approach which also improves recovery. This further reduces the costs and complications associated with postoperative opioid use. These are all pieces of the puzzle for improving outcomes and lowering costs."
Dr. Wang's non-narcotic multi-modal approach to pain management includes:
• Use of endoscopic access and expandable cages to minimize tissue trauma during surgery
• Using EXPAREL and other local anesthetics such as Marcaine and epinephrine when placing percutaneous pedicle screws and rods (replaces patient-controlled analgesia with morphine)
• Carefully-monitored anesthesia during the procedure without endotracheal intubation
Dr. Wang's study compared outcomes associated with open TLIF versus MIS TLIF and found that patients who underwent MIS TLIF experienced shorter time-to-discharge, reduced hospital charges and lower transfer rates to inpatient rehabilitation.
Building on his 2009 findings, Dr. Wang assessed the same outcome measures associated with an awake MIS TLIF procedure, and found cost savings of approximately $20,000 per procedure, and the length of stay shortened by two to three days. In addition, Dr. Wang also found improvements in patient satisfaction and return to function.
Table 1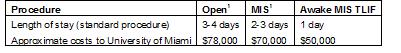
Dr. Wang credits his ability to perform awake MIS TLIFs in part to EXPAREL, which he refers to as a "game-changer" for select spine surgeries. Last fall, Dr. Wang’s colleague, Karthik Madhavan, MD, of the University of Miami, presented data from an independent pilot study at the North American Spine Society annual meeting evaluating the use of EXPAREL on one- to two-level open spine surgeries.
Dr. Madhavan evaluated 16 patients who received either liposomal bupivacaine (expanded with preservative-free saline to 40-60 cc) or Marcaine 0.25 percent with epinephrine prior to closure. Inclusion criteria specified that enrolled patients should not be using narcotics preoperatively. Dr. Madhavan measured pain scores (1-10), narcotic consumption, and postoperative movement for more than 150 feet and found that patients who received liposomal bupivacaine consumed up to 50 percent fewer narcotics and reported pain scores an average of four points lower than their counterparts. In addition, five out of the eight patients who received liposomal bupivacaine were able to walk 150 feet, compared to two out of the eight patients in the Marcaine group, at the same postoperative time point. Further, a blinded nurse practitioner was able to identify the patients who had received liposomal bupivacaine.
As a result, Dr. Madhavan concluded, "EXPAREL is very effective in reducing postoperative pain in this pilot investigation. Furthermore, as the drug does not diffuse into the tissues, more surgical area should be covered with injections using a specific technique."
In September 2014, at the annual meeting of the Society for Minimally Invasive Spine Surgeons (SMISS), William Tally, MD, a spine surgeon at Athens (Ga.) Orthopedic Clinic, presented data evaluating the efficacy and safety of EXPAREL in spine procedures performed in an ambulatory surgery center setting. Dr. Tally assessed 46 patients who underwent either an MIS TLIF or a midline laminectomy, and were given EXPAREL for postoperative pain.
Key findings were:
• No adverse events including spinal anesthesia and nerve blocks
• No transfers to inpatient status
• No wound complications
• All patients were discharged home on the day of surgery
• All patients were discharged with oral NORCO (5/325 1–2 tablets prn) and oxycodone (5mg) for breakthrough pain as well as Flexeril (10 mg) and Valium (5 mg) PRN for muscle spasms
--
Wang, Michael Y., et al. "An analysis of the differences in the acute hospitalization charges following minimally invasive versus open posterior lumbar interbody fusion: Clinical article." Journal of Neurosurgery: Spine 12.6 (2010): 694-699.


