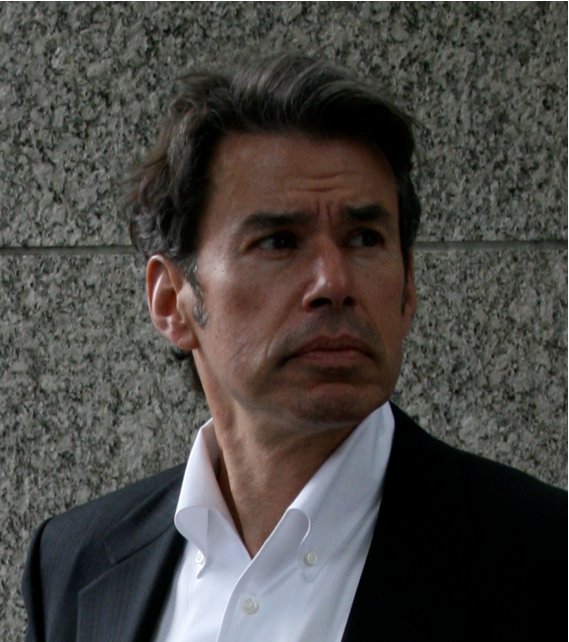
 Richard Wohns, MD, JD, MBA, founder of NeoSpine in the Puget Sound Region, Washington, discusses five areas where spine surgeon leaders must focus their guiding attention in the future.
Richard Wohns, MD, JD, MBA, founder of NeoSpine in the Puget Sound Region, Washington, discusses five areas where spine surgeon leaders must focus their guiding attention in the future.
1. Lead the charge to more integrated spine care. Healthcare has become more integrated and the most cutting-edge physician leaders are now transforming their practice into a multidisciplinary setting. Incorporating multiple spine specialists allows surgeons to coordinate care more easily for patients, whether they need imaging, nonoperative treatment or surgery.
"I firmly believe in the integrated model of spine care," says Dr. Wohns. "You cannot operate in a vacuum. The best practices have an integrated model where the spine surgeon has put together specialists in the practice that they collaborate with on a daily basis for a majority of their patients."
Committing to nonoperative treatment as well as surgery in appropriately indicated patients shows the desire to provide a variety of treatment options.
"Spine surgeons now need to recognize that the paradigm is very much changed from the past and they have to adjust their practices to the fact that more surgeries are being scrutinized by the government, payers and the media," says Dr. Wohns. "Whether or not spine surgeries are clearly indicated and necessary, spine surgeons have to realize that they are in the cross hairs of a variety of these powerful entities. We need to be proactive in educating the rest of the world to recognize how our minimally invasive and outpatient treatments provide good outcomes and results, and are cost effective. We need to show that what we do creates value for patients and the other stakeholders in the healthcare delivery system."
2. Develop minimally invasive and outpatient procedures. Spine surgery is gradually moving into the outpatient setting for a variety of reasons, including:
• New and enabling surgical technologies
• Improved anesthesia regimens
• Lower infection rate
• Shorter length of stay
• Quicker recovery times
• Higher patient satisfaction
• Less costly care.
As technology develops allowing spine surgeons to perform a wider variety of cases with minimally invasive procedures, surgeons at the cutting edge will be blaze the trail to better care for their patients.
"People are being trained more in the realm of minimally invasive spine surgery and outpatient procedures," says Dr. Wohns. "It's becoming more of a standard practice. In some areas, insurance companies are telling providers they will only approve outpatient procedures for spine surgery, which is a big change from 10 years ago."
Insurance companies have realized the cost-savings and quality of care available in the outpatient setting and are excited about working with surgeons and ASCs to transition the appropriate cases.
3. Engage in efforts to control the cost of care. Cost containment is one of the reasons insurance companies are denying spinal surgery at a higher rate than before. However, for patients who don't benefit from conservative treatment, global costs overtime from nonoperative care will exceed the one-time cost of an effective surgery.
"By virtue of the denial, they save a dollar that day, but there are unintended consequences of this policy," says Dr. Wohns. "They might deny surgery for a patient with a degenerative condition who needs surgery to prevent additional decline. Then the patient worsens and the condition doesn't go away with conservative treatment."
The patients then expend healthcare dollars for a variety of non-curative, non-surgical care options, during which time the degenerative cascade relentlessly progresses "That dollar saved today increases overall healthcare expenses for the future because when patients are denied appropriate surgery based on medical necessity and evidence-based medicine, it's inevitable they'll eventually need more care," says Dr. Wohns. "That's important for surgeons to recognize and vocalize to payers and the government. We need to tell them as patient advocates that denial of care will increase costs going forward."
4. Organize a response to care denials. Nearly every spine surgeon has experienced an increasing rate of denials, whether seeking approval for a surgical case or payment after the procedure. Today's leaders must advocate swiftly with insurance companies to ensure these treatments are appropriately covered in the future.
"We need to be much more organized in our response to denials, insurance companies and the media," says Dr. Wohns. "Every practice puts together their appeal package and deals with payers. Because of the prevalence of evidence-based medicine and articles to support most surgeons' decision making and guidelines, we should have a better organized, proactive list of why we are making these decisions instead of just stating the treatment is indicated based on radiological findings and symptoms."
National and local medical and spine-focused organizations are leading efforts to respond when insurance companies review coverage policies for spinal procedures. Participate or financially support these efforts to invest in the future of your practice.
5. Promote appropriate treatment guidelines. Many insurance companies use the Milliman guidelines as a basis for coverage decisions. However, these guidelines are based on weak and outdated studies, and ignore recent literature in favor of surgical intervention in some situations.
"We must template out the appropriate literature and guidelines that need to be cited and recognize what the adverse respondents are going to say," says Dr. Wohns. "Like in martial arts, know what they are going to say before they launch their offensive: a strong defense is a strong offense."
At the local level, individual groups must also develop protocols to move patients quickly through a treatment algorithm. Decide which pathways patients will follow and make sure all specialists are in agreement.
"You want everyone one the same page," says Dr. Wohns. "Create algorithms for care pathways for the various types of spine patients. Sometimes there is a shift in how you take care of people because nothing is 100 percent the same every time, but if you have the general framework, it really streamlines care."
More Articles on Spine Surgeons:
The Long-Term Fulfillment in a Spine Surgeon's Career: Q&A With Dr. William Watters of The Baylor College of Medicine
5 Pillars of Independent Spine Groups Today
Driving Value in Spine Care: Outpatient Spine Surgery


