Pressures from patients and the healthcare system at large for shorter hospitalization, quicker return to function, and reduced overall expense demand that today's spine surgeon develop expertise in anatomy conserving surgical techniques. The conservation of anatomy by limiting incision, dissection, and retraction can reduce post-operative morbidity and profoundly impact these metrics.
Sponsored by Spineology.
An evolving anatomy conserving stabilization method which uses a small midline incision, interbody fusion (IBF), and a divergent, corticocancellous screw trajectory has been gaining in popularity.
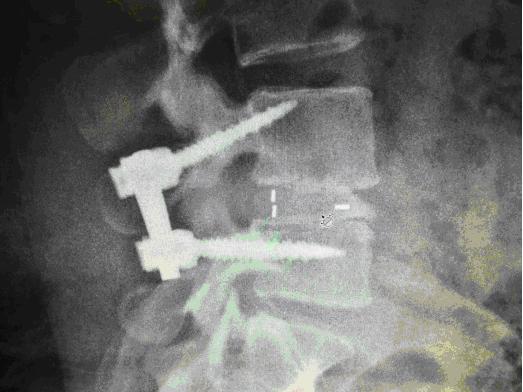

Photos: Patient treated with MediaLIF construct
This increase in popularity can be attributed to numerous factors, including:
1. Stabilization quality: The use of interbody fusion provides excellent anterior column support and the screw trajectory engages more cortical bone than traditional approaches.
2. Decompressive access: The procedure is done through a midline (laminectomy) exposure and provides excellent visualization of all neural anatomy.
3. Anatomy conservation: Construct assembly can be completed within the confines of a typical laminectomy exposure; no additional exposure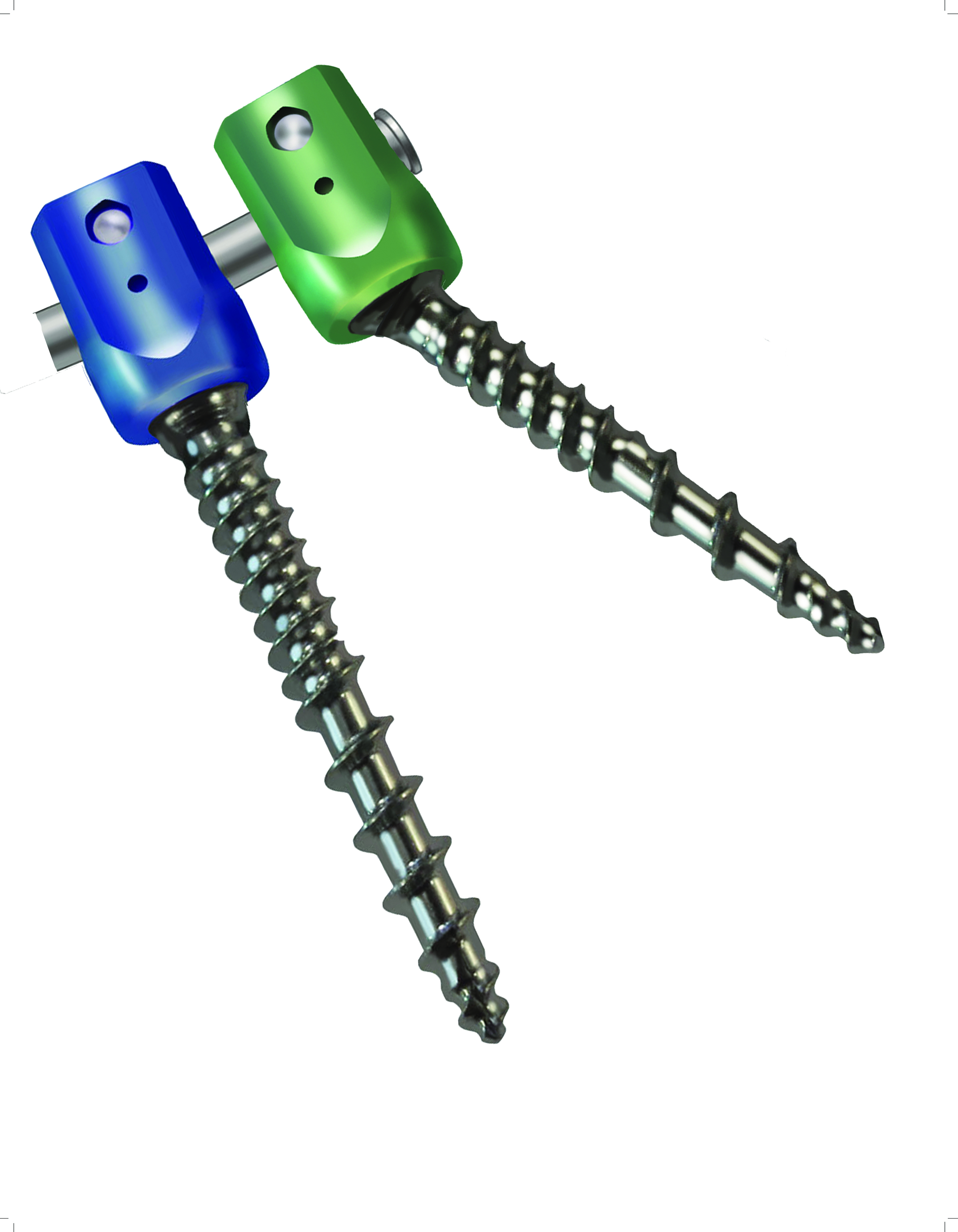 for the fusion construct is required. This greatly limits incision size, dissection and retraction.
for the fusion construct is required. This greatly limits incision size, dissection and retraction.
4. Procedural efficiency: Limiting dissection and improving decompression visibility can greatly decrease procedure time. In addition to being beneficial for the patient, this can benefit all aspects of healthcare delivery. Day surgery application is also possible.
5. Broad utility: As a result of the direct decompressive access and the quality of the stabilization achieved, this technique is applicable to most lumbar fusions.
Due to these advantages, I have altered my preferred fusion methodology and have experienced what I consider to be good to excellent clinical results. In my own practice, I have experienced a reduction in postoperative morbidity leading to a reduction in hospital stay from three days to one day.
The technology
Using divergent screw trajectories causes the screw tulips to be medial and in close proximity. As such, the screw head design needs to be as small as possible to limit crowding, simplify assembly and above all avoid adjacent level impingement.
Screw shank design is also important. With the increase in cortical engagement, a tapered tip with a self-tapping feature can be very helpful in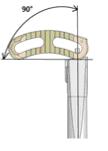 screw starting and advancement. Additionally, because of the trajectory variation, 4.5mm diameter screws as short as 25mm in length, that retains as much cross section as possible in the neck, are a requirement.
screw starting and advancement. Additionally, because of the trajectory variation, 4.5mm diameter screws as short as 25mm in length, that retains as much cross section as possible in the neck, are a requirement.
Cage design for a medial IBF implantation also has special requirements. While a traditional PLIF lends itself nicely to this procedure, it is also common for surgeons to use a single implant technique (ex. TLIF) as it only requires the exposure of a single nerve root. The new generation of articulating curved TLIF cages lend themselves nicely to this procedure. Due to the vertical (PA) or even divergent nature of the exposure, however, using a device that can be articulated to a full 90 degrees is important.
When using traditional open pedicular fixation methods, the lateral-to-medial screw trajectory demands a large incision and wide retraction to place screws. When using a divergent angle screw trajectory the incision size is greatly reduced. This requires a retractor specifically designed for the medial approach. The key design feature is the blade toeing capability, as it greatly limits incision size, dissection, and retraction, while still providing excellent visualization.
The learning curve for placing corticocancellous screws and interbody devices through a medial approach is relatively short compared to other minimally invasive procedures. This is directly attributable to the direct visualization provided by the approach and most surgeon's familiarity with other posterior procedures and landmarks used to target and place screws and cages.
minimally invasive procedures. This is directly attributable to the direct visualization provided by the approach and most surgeon's familiarity with other posterior procedures and landmarks used to target and place screws and cages.
Photos from Spineology Inc. St. Paul, MN
Fortress Pedicular Fixation System
Rampart T Interbody fusion system
Medicus Retractor System


