Committed to revolutionizing minimally invasive neurosurgery, NICO Corp. disrupted the industry with a set of technologies and a standardized surgical approach that allows neurosurgeons to do the presumed impossible, while at the same providing impressive economic benefits to the hospital.
"Neurosurgeons are identifying more and more cases and disease states where our technologies can be used to help appropriate patients in a very positive way," says Jim Pearson, president and CEO of the Indianapolis-based corporation. "In many of the published instances, these cases were considered inoperable before. Now, they can be surgically managed with our technologies, and it's giving more patients a sense of hope where there was none before."
The BrainPath technology was cleared by the FDA in 2012 and granted additional disease state specific indications in 2016 for use on primary and secondary tumors and intracerebral hemorrhages. Before the technology's introduction, many tumors and brain-bleed conditions possessed no effective surgical option.
BrainPath provides non-disruptive access and improved visualization of lesions situated in the brain's subcortical area. Unlike previous technologies, BrainPath does not cut through white matter, but moves along the brain's natural folds and fibers to limit tissue damage and give the patient improved odds for a faster recovery with fewer deficits.
The technology is navigable and features a uniquely engineered tip and side vents that allow equal dispersion of tissue as it moves to the target site. Once surgeons take out the obturator, an outer sheath stays intact to provide a small working corridor to the surgical site.
While BrainPath and Myriad, a NICO technology used for tissue removal without using heat, are the lead technologies in safely reaching the abnormality and removing it, they are used in combination with other technologies to be part of a systems approach to brain surgery. "We work in collaboration with other imaging technologies that enable surgeons to see what they want to get, and then our technologies help them get what they see without the typical associated damage to healthy brain tissue," says Mr. Pearson.
The systems approach is known in the industry as the BrainPath Approach, and evidence of both clinical and economic benefits have been collectively published in 50 papers, posters and abstracts.
"We also have a new published paper that reveals an average economic benefit to the hospital of $11,773 per patient or a net estimated benefit of $329,659 resulting from fewer ICU days and the ability to provide surgery for patients that previously would not have been candidates," adds Mr. Pearson. "This is of significant interest to hospital administrators and with non-disruptive access to the brain, we are finally achieving the last major medical revolution in minimally invasive surgery."
Clinical and economic benefits
The BrainPath Approach features three key components: access, removal and tissue collection/preservation.
1. Non-disruptive access. NICO hopes to prove the shortest route is not always the safest route for brain tumor removal or hemorrhage evacuation. BrainPath represents the world's first and only trans-sulcal technology, requiring the surgeon to access the brain via a trans-sulcal approach and, in some cases, transverse more brain; this approach is much like in cardiac surgery when stents traveled up the leg to reach the heart versus opening the chest for access, which was the shorter but more damaging route.
"This parallel shows how improved outcomes revolutionized cardiac surgery when minimally invasive access was combined with advanced imaging," explains Mr. Pearson. "The first step of access is combining intervention with imaging and tractography, so we can see where we want to go, navigate the path and get there without damaging brain tissue."
2. Removal. Tumor removal and clot evacuation are accomplished using the automated NICO Myriad. Hitachi Aloka also makes the BrainPath ultrasound probe that provides a critical missing link of real-time visualization while positioned down the small BrainPath corridor.
"You need ultrasound and imaging, so the BrainPath ultrasound probe is real-time imaging coupled with intervention to effectively get the tumor out or remove blood in a hemorrhagic stroke with little or no trauma to the patient," Mr. Pearson says.
3. Tissue collection. The final step in the BrainPath Approach involves intraoperative collection and preservation of the tumor tissue. The automated process of removal and collection allows pathologists to treat the tissue like a discrete organ, preserving it to provide opportunities for using the tissue for personalized medicine options or other research once the brain surgery is complete.
Published research has indicated patients undergoing BrainPath Approach surgery have a 50 percent decrease in hospital length of stay, as well as significantly reduced deficits that result in accelerated recoveries. These benefits are part of what contribute to the economic benefits of the approach, which were featured in a recent published economic study from a single university hospital in the Midwest that found a greater than 50 percent average reduction in intensive care unit length of stay for patients with brain tumors and hemorrhagic stroke.
"There were two big themes [from the economic study]," notes Craig Blanchard, NICO vice president of marketing and field clinical. "Costs were reduced as a proxy with BrainPath in the ICU, shortening length of stay in the ICU from 11 days to four days. The other important element is more patients were deemed clinically appropriate to be surgically treated – giving them a surgical option they would not have had in the past."
Who's using the BrainPath Approach and technology?
Approximately 125 institutions are currently using the BrainPath Approach, including about 80 percent of major academic medical centers in the U.S. More than 7,000 procedures have been performed using BrainPath and over 12,000 Myriad procedures.
Kaisorn Chaichana, MD, an assistant professor of neurosurgery at Baltimore-based Johns Hopkins, is one such user. He has been using the BrainPath Approach for three years, using the technologies in about 50 cases for tumors situated deep inside the brain, as well as cranial hemorrhages.
"The tubular retractor system allows you to go in between the natural grooves of the brain," Dr. Chaichana says. "I can go in and out of very dangerous locations with minimal risks."
Dr. Chaichana says he recommends BrainPath to other neurosurgeons, labeling it a great technology.
NICO is far from done with innovation. The company plans to introduce its newly cleared technology that is the world's smallest and only trans-sulcal access system for brain surgery and a tool for hemostasis management in early 2018. NICO is also in the midst of a randomized controlled clinical trial evaluating the benefits of early evacuation of ICH as compared to standard medical management. The ENRICH trial will encompass 300 patients and 30 healthcare centers, including Johns Hopkins.
Hear a patient testimonial, here.
BrainPath Approach technology and Myriad

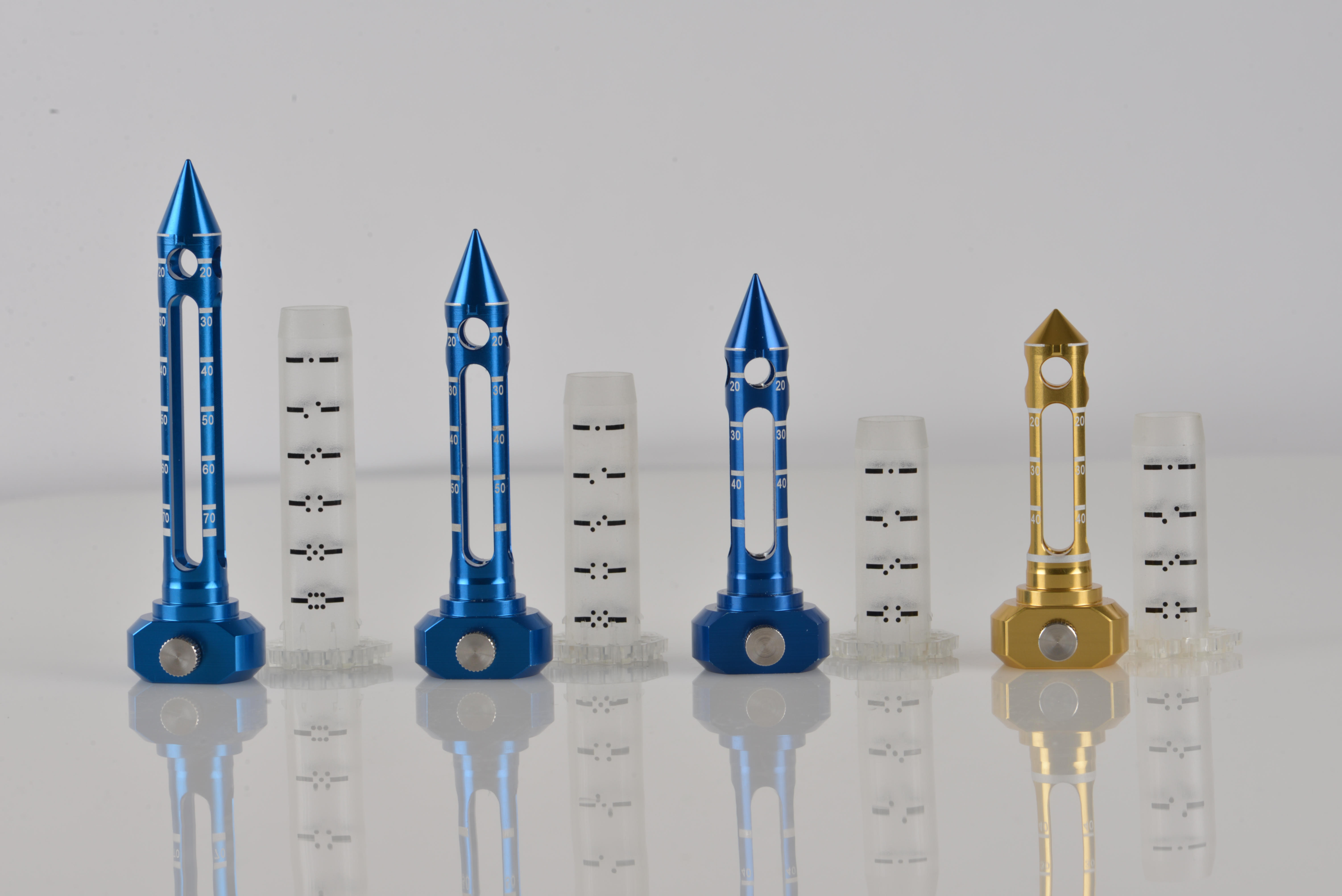
The new 11 mm BrainPath family of products, the smallest tool in the world for trans-sulcas access for brain surgery

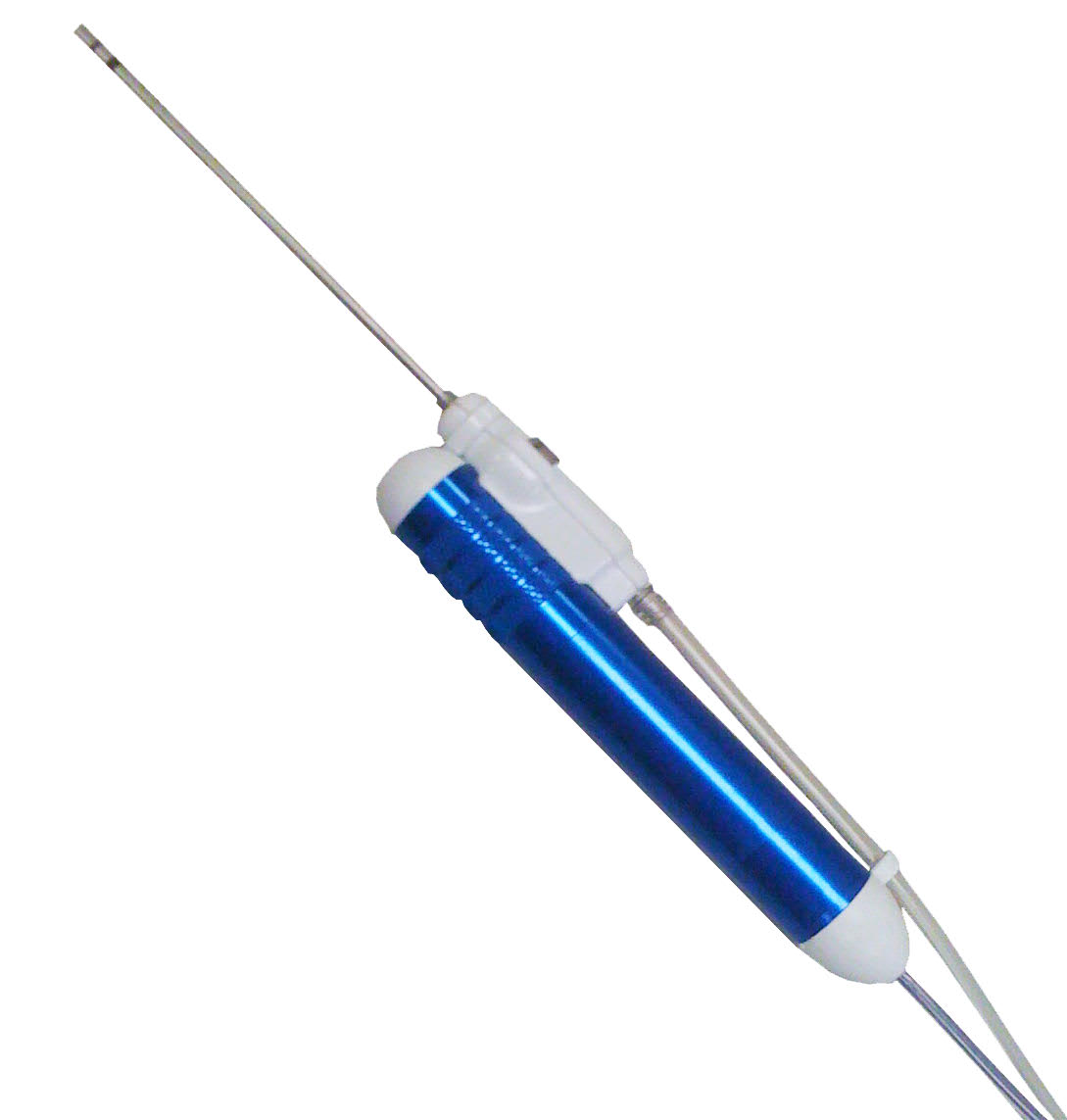
The new TRIOwand, used in the removal step of the BrainPath Approach for irrigation, variable suction and coagulation in one tool to achieve hemostasis at low wattage and preservation of nearby eloquent tissue.


